Vaginal Bleeding: Causes, Symptoms, Diagnosis & Treatment
Per vaginal (PV) bleeding refers to any bleeding from the vagina that is not part of a normal menstrual period. It can occur in women of all ages and may be a sign of a minor issue or a more serious underlying condition. Prompt evaluation is essential to determine the cause and ensure appropriate treatment.
CAVEATS
- For the majority of women this presentation is indicative of a menstrual disturbance which can be adequately controlled with simple outpatient treatment prior to a gynaecological review.
- Unexpected bleeding may be a complication in early pregnancy, while a minority of women encountering vigorous or prolonged bleeding may already be haemodynamically compromised at the point of consultation.
- The preliminary assessment should focus on recognizing the woman who requires resuscitation, identifying the source of bleeding (and determining the pregnancy status), and initiating the appropriate management.
Clinical Assessment
Assessment of patient with abnormal vaginal bleeding
Age : reproductive age group, perimenopausal or postmenopausal.
Medical history: previously diagnosed pelvic inflammatory disease or sexually transmitted infections (in particular, gonorrhoea and chlamydia), use of anticoagulants, coagulopathy, unopposed oestrogens, postmenopausal hormone therapy, or tamoxifen.
Surgical history: recent hysterectomy, or vaginal or other pelvic surgery.
Significant drug history: warfarin or other anticoagulants.
Gynaecological symptoms:
- Parity and obstetric history.
- Menstrual cycle: regularity, date of last normal menstrual period.
- Contraceptive use: combined oral contraceptive pill, progesterone-only implant or injections,
intrauterine device, and if the patient is on hormonal contraception whether she has deviated
from her schedule. - Bleeding characteristics: number of episodes, duration, volume, and previous treatment.
- Abdominal or pelvic pain.
- Symptoms of early pregnancy.
- Symptoms of chronic anaemia.
Physical examinatioп
- Haemodynamic instability.
- Abdominal examination (for evidence of intraperitoneal bleeding): abdominal tenderness with/ without rebound tenderness and guarding; pelviabdominal mass (suggestive of gravid uterus).
- Pelvic examination:
- Speculum examination (to identify the source and magnitude of bleeding): from the uterus
(blood discharged through the cervical canal), cervix (from local lesions or tumours),
vagina and vulva (trauma or lesions), or extragenital bleeding from the urethra/anus. - Bimanual examination: external cervical os (opened or closed); uterine size, mobility, and tenderness; adnexal masses and tenderness (possible ectopic pregnancy).
- Speculum examination (to identify the source and magnitude of bleeding): from the uterus
Diagnostic investigations
- The following are usually performed by the gynaecologist:
- Pelvic ultrasonography (transvaginal, TVUS; or transabdominal, TAUS).
- Endometrial biopsy where indicated.
SPECIAL TIPS FOR GPs
- Perform a urine pregnancy test (UPT) for all women in the reproductive/premenopausal age
- group, regardless of menstrual pattern or the reported last menstrual period.
- Perform GXM if the patient is likely to require an urgent transfusion.
- Check FBC and coagulation profile.
Management
Haemodynamically unstable patients
- Consult the gynaecologist immediately.
- Secure IV line and initiate fluid resuscitation.
- Perform a UPT to confirm pregnancy.
- Consider CBD for fluid monitoring.
- Investigations: FBC, GXM, and coagulation profile (optional).
If the patient is pregnant:
- A ruptured or bleeding ectopic pregnancy must be excluded. The gynaecologist will perform a TVUS to determine if there is an intrauterine gestational sac, fluid in the peritoneal cavity, and/or an adnexal mass suggestive of a haemorthaging ectopic pregnancy. When this is confirmed the patient needs to be admitted and prepared for emergency surgery.
- Differential diagnosis: haemorrhage from a miscarried intrauterine pregnancy.
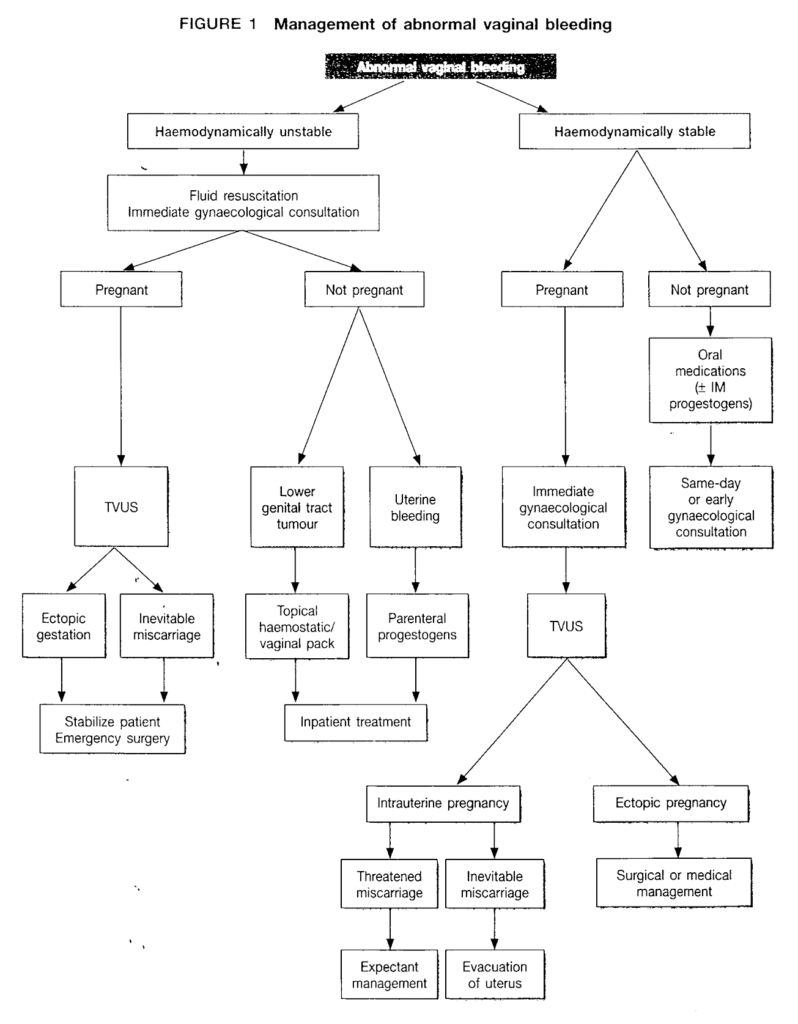
FIGURE 1: Management of abnormal vaginal bleeding
If the patient is not pregnant:
- Differential diagnoses:
- Menstrual disorders
- Endometrial hyperplasia (e.g. anovulatory cycles with a current episode of prolonged and heavy uterine bleeding)
- Lower genital tract malignancy (consnonly cervical or endometrial tumours).
- Genital tract trauma (e.g. postcoital vaginal laceration, cervical cone biopsy).
Acute management is cause-specific:
- Once pregnancy and a lower genital tract lesion are excluded, abnormal uterine bleeding
can be controlled with a single administration of IM progesterone (100-200 mg), or IM
Provera (150 mg). - Local bleeding from a cervical tumour or cone biopsy site can be controlled with the topical application of a haemostatic agent, such as Monsel’s solution (ferric subsulphate, usually available as a paste and applied with a Q-tip), a painless and effective means of achieving haemostasis.
- Small bleeders on the surface of the cervix can be accurately cauterized using silver nitrate (available as a solid pencil to facilitate topical application). Alternatively, a vaginal pack (lubricated with saline and with the tip soaked in tranexamic acid) may be applied to tamponade the bleeding.
- If there is vigorous bleeding from the surface of a cervical tumour, consider the use IV tranexamic acid as a slow bolus (500-1000 mg).
- The patient should be stabilized, admitted, and investigated adequately before definitive treatment is administered.
Haemodynamically stable patients
If the patient is pregnant:
- Bleeding in the first trimester may be caused by an ectopic pregnancy; this must be excluded by TVUS. Other possible causes of early gestational bleeding include a threatened or inevitable miscarriage.
- Vaginal bleeding in advanced gestation is known as antepartum haemorrhage and common causes include placental abruption and placenta praevia. In any situation, initially modest bleeding may quickly escalate in volume and vigour, leading to haemodynamic compromise. Thus, serial monitoring and immediate or same-day gynaecological review is important.
If the patient is not pregnant:
- Menstrual disorders (e.g. menorrhagia, polymenorrhoea, anovulatory cycles with prolonged
menstrual bleeding). - Endometrial hyperplasia.
- Genital tract lesions (e.g. cervical or endometrial malignancies) or trauma.
- Postmenopausal bleeding due to atrophic endometritis/cervicitis/vaginitis.
Cervical tumours are identified on speculum examination. Local bleeding can be controlled with the application of haemostatic agents or a vaginal pack (as described earlier). A same-day gynaecological review should be arranged.
If the patient has recently had uterine, cervical, or vaginal surgery and the bleeding is suspected to originate from the operative site, immediate gynaecological review should be arranged. An episode of heavy uterine bleeding can be controlled with the administration of IM progesterone (100-200 mg) or IM Depo-Provera (150 mg) followed by oral norethisterone (10 mg three times daily) continuously until the patient is reviewed by the gynaecologist.
If the bleeding episode is moderate the patient may be started on oral medications directly. The options include tranexamic acid (1000 mg two to four times daily), non-steroidal anti-inflammatory medications, e.g. mefenamic acid (500 mg three times daily), or progestogens (e.g. norethisterone 10 mg three times daily). An early gynaecological referral should be arranged for a complete assessment before definitive treatment is offered. Medications are to be continued until the patient is reviewed.
References
- National Institute for Health and Clinical Excellence. Heavy menstrual bleeding. NICE Clinical Guideline 44. 2007.
- Royal College of Obstetricians and Gynaecologists. The management of tubal pregnancy. Green-top Guideline No. 2004.
- Jetmore AB, Heryer JW, Conner WE. Monsel’s solution: A kinder, gentler hemostatic. Dis Colon Rectum. 1993; 36(9): 866-867.
- Grimes DA, Hubacher D, Lopez LM, Schulz KF. Non-steroidal anti-inflammatory drugs for heavy bleeding or pain associated with intrauterine-device use. Cochrane Database Syst Rev. 2006(4): CD006034.
- Lethaby A, Augood C, Duckitt K, Farquhar C. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007(4): CD000400.
- Lethaby A, Irvine G, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000(2): CD001016.
- Coulter A, Kelland J, Peto V, Rees MC. Treating menorrhagia in primary care. An overview of drug trials and a survey of prescribing practice. Int J Technol Assess Health Care. 1995; 11(3): 456–471.