Approach To Abdominal Pain
Abdominal pain is a common symptom that can range from mild discomfort to severe, life-threatening conditions. It can originate from various organs within the abdomen or from related structures and requires careful evaluation to determine the cause.
Approach To Acute Abdomen
Definition: the presence of an abdominal pathology which if left untreated (<72 hours) will
result in patient morbidity and mortality.
Sudden onset of severe abdominal pain (new pain or an increase in chronic pain) is the hallmark
of the acute abdomen
Most common general surgical problem presenting to the emergency department
Abdominal Pain arising from intra-abdominal pathology originates in the peritoneum (visceral
and parietal layer)
A transition from visceral to somatic pain indicates extension of the underlying process
TABLE 1 Potentially life-threatening causes of abdominal pain
| Intra-abdominal | Perforated peptic ulcer Intestinal obstruction AAA/aortic dissection Appendicitis Pancreatitis Ectopic pregnancy Ischaemic bowel Peritonitis: spontaneous bacterial peritonitis in liver cirrhosis, peritoneal dialysis related Hepatobiliary sepsis |
| Extra-abdominal | Acute myocardial irifarction (AMI) Lower-lobe pneumonia Basal pulmonary embolism Diabetic ketoacidosis Systemic lupus erythematosus (SLE) vasculitis |
Life Threatening Conditions Of Abdominal Pain in Adults
1. Perforated Viscus (i.e. perforated peptic ulcer most common)
- Patient tends to be in the younger age group (20-30)
- Can presents to ED, 2-3 days after onset of epigastric pain
- Suspected in individuals with hx of PUD symptoms and who develop sudden onset of severe, diffuse abdominal pain
- Others causes includes:
- Perforated oesophagus (Boerhaave syndrome)
- Perforated bowel (ischemic bowel, toxic megacolon, diverticulitis)
- Perforated appendix
2. Ruptured Abdominal aortic aneurysm (AAA)
- Risk Factors: advanced age (>60 years). COPD, pulmonary disease, PVD, HTN, smoking and family history
- Hallmark: pulsatile epigastric mass, if ruptured exsanguinating haemorrhage, unstable hypotension
3. Mesenteric Ischemia
- Risk Factors: advanced age, ATH, low cardiac o/p state, cardiac arrhythmias (i.e. AF), severe cardiac valvular disease, recent AMI, intra-abdominal malignancy
- Hallmark: acute onset of severe periumbilical abdominal pain out of proportion to findings on physical examination
4. Acute Bowel Obstruction (i.e. small bowel obstruction most common)
- Hallmark: crampy abdominal pain, abdominal distention, obstipation, vomiting -> progression of pain from crampy to constant and more severe can be a sign of impending strangulation
5. Severe Pancreatitis
– Unless it is haemorrhagic pancreatitis (rare on 1st presentation)
6. Ruptured HCC
7. Medical Conditions
- Diabetic Ketoacidosis
- Acute MI
- Addison’s Disease (Addisonian crisis)
8. Obstetric Conditions
- Ruptured Ectopic Pregnancy
- Placental Abruption
The chest X-ray is utilized to identify the following:
- Subdiaphragmatic air.
- Basal consolidation.
- Pulmonary embolism (ruling out other lung pathologies).
SPECIAL TIPS FOR GPs
- The site and nature of the abdominal pain will give the best clue as to what is causing it.
- Always suspect ectopic pregnancy in women of child-bearing age.
- Always suspect appendicitis in any man with lower abdominal pain.
- Do not forget to feel for epigastric pulsation and check all pulses to look for AAA and aortic dissection respectively.
- Myocardial infarction may give upper abdominal pain. Perform an ECG.
Physical Examination
General Appearance
– Lying motionless (Acute Appendicitis, Diffuse Peritonitis)
– Restless, writhe in pain (Ureteric Colic, Intestinal Colic)
– Bending Forward (Pancreatitis)
Vital Signs + Peripheral Signs
– Hemodynamic Instability – r/o life threatening causes of epigastric pain
– High Grade Fever – suggests abscess, cholangitis or pneumonia
– Peripheral signs: jaundice, pallor, peripheral vasoconstriction, hydration status
Abdominal Examination
Inspection (from the foot of the bed)
– Distension, Surgical Scars, Bulging Masses, Area of erythema, Pulsations, Peristalsis
Palpation (patient in supine position, eyes fixed on patient’s eye)
– Peritoneal Signs – rebound tenderness, guarding, board-like rigidity
– Any palpable masses
– Hernias – incisional, ventral, umbilical, inguinal, femoral
– Pain out of proportion to PE findings – suggest mesenteric ischemia
Percussion
– Dullness over bladder – acute urinary retention
– Tympanic sounds over distended bowel – intestinal obstruction
Auscultation
– Absence of bowel sounds – possibly ileus from diffuse peritonitis
– High-pitched tinkling bowel sounds – suggestive of obstruction
Rectal Examination
Testicular and Scrotal Examination
Others
– Peripheral vascular signs of embolization
– Evidence of coagulopathy
Investigations
Blood
- Full Blood Count
- Renal Profile
- Hypokalemic, Hypochloremic and Metabolic Alkalosis – prolonged vomiting and severe volume depletion
- (gastric outlet obstruction) – a/w high urea and creatinine if patient is dehydrated
- Low Serum Bicarbonate or Metabolic Acidosis – ? general tissue hypo-perfusion (intestinal ischemia)
- HypoK+ / HypoCa2+ can cause ileus, third spacing can also cause electrolyte imbalance
- Cr – for suitability of contrast scans
- Glucose – to exclude DKA
- Liver Function Test (LFTs)
- Hepatitis vs. obstructive vs. mixed picture
- Pancreatic Enzymes (amylase and lipase)
- Serum amylase peaks at 6-24 hours (if > 3x normal limits) suggestive of acute pancreatitis.
- Amylase can also be raised in perforated viscus, IO, ischemic bowel, ectopic pregnancy
- Cardiac Enzymes (CK/CKMB/Trop T), ECG – tro ACS
- Lactic Acid Level (consideration of intestinal ischemia)
- Serum lactate as an indicator of tissue hypoxia (suggestive of mesenteric ischemia or worsening sepsis)
- UFEME
- UPT
GXM / PT/PTT – if surgery required
Radiological Investigations
Plain Abdominal X-Ray Series
– Erect Chest X-Ray – look for free air under the diaphragm (diff dx: Chilaiditi syndrome)
Supine Abdominal X-Ray or KUB
– Free air distribution throughout Small Bowel (jejunum – valvulae conniventes) and Large Bowel (haustrations)
– Coffee Bean Sign (‘bent inner tube’ – indicative of sigmoid volvulus)
– Calcifications – most urinary stones are radio-opaque (90%), only 15% of gallstones are calcified
– Sentinel Loop in acute pancreatitis
– Calcification in the pancreas – chronic pancreatitis
– Ground glass appearance – ascites
– KUB – can look for rectal gas (beware of the presence of colonic gas following DRE)
Erect Abdominal X-Ray (not routine)
– look for air-fluid level (5 or more is diagnostic for intestinal obstruction)
Ultrasonography
– Can detect up to 95% of gallstones
– Acute Cholecystitis – diagnosed via (1) thickened gallbladder wall (>3mm), (2) pericholecystic fluid, (3)
stone impacted at neck of gallbladder and (4) sonographic murphy’s sign
CT Scan
– Evaluate acute mesenteric ischemia with CT angiography
– Good for evaluating retroperitoneal structures – suspected leaking AAA or nephrolithiasis
Magnetic Resonance Imaging (MRI)
– Greatest application in pregnant women with acute abdominal and pelvic pain
Management
Haemodynamically unstable patient
- The patient must be managed in the critical care area.
- Maintain the airway and give supplemental high-flow oxygen.
- Monitoring: ECG, vital signs q5 minutes, and pulse oximetry.
- Establish 2 large-bore peripheral IVs (14-16 g); fluid challenge of 1-2 L of crystalloid (if AMI is not suspected). Reassess parameters.
Labs:
– Mandatory: capillary blood sugar; GXM 2 to 4 units; FBC; urea/electrolytes/creatinine;
liver function tests (LFTs); serum amylase; urine pregnancy test (where relevant); and first
blood and urine cultures (if sepsis is suspected).
Optional: urinalysis, cardiac enzymes, LFTs, and coagulation profile.
IV antibiotics in cases of intra-abdominal sepsis, e.g. ceftriaxone 1 g and metronidazole 500
mg. Depending on local practice, other antibiotics to cover Gram-negative and anaerobic
organisms can be used.
X-rays: CXR and kidneys, ureters, bladder (KUB) X-ray.
ECG to identify AMI or as preparation for anticipated surgery in suitable age groups.
Insert CBD
Keep the patient nil by mouth.
- Early consultations with, e.g. the following:
- General surgery registrar.
- Obstetrics and gynaecology registrar for suspected ectopic pregnancy.
- Cardiothoracic registrar for suspected abdominal aortic aneurysm.
- Medical or cardiology regištrar for suspected basilar pneumonia or myocardial infarction.
Haemodynamically stable patient
- This patient can be managed in the intermediate acuity area.
- Keep the patient nil by mouth till disposition has been decided.
- Consider a precautionary intravenous plug.
- Labs should be based on clinical suspicion of the possible causes of abdominal pain in a particular patient.
- Consider KUB, CXR, and ECG.
- Evaluate for signs of acute abdomen with frequent abdominal examinations.
- At one time it was believed that analgesia interferes with the assessment of patients with
abdominal pain. Many studies have disproved this idea; patients with abdominal pain should
be treated judiciously with appropriate analgesics.
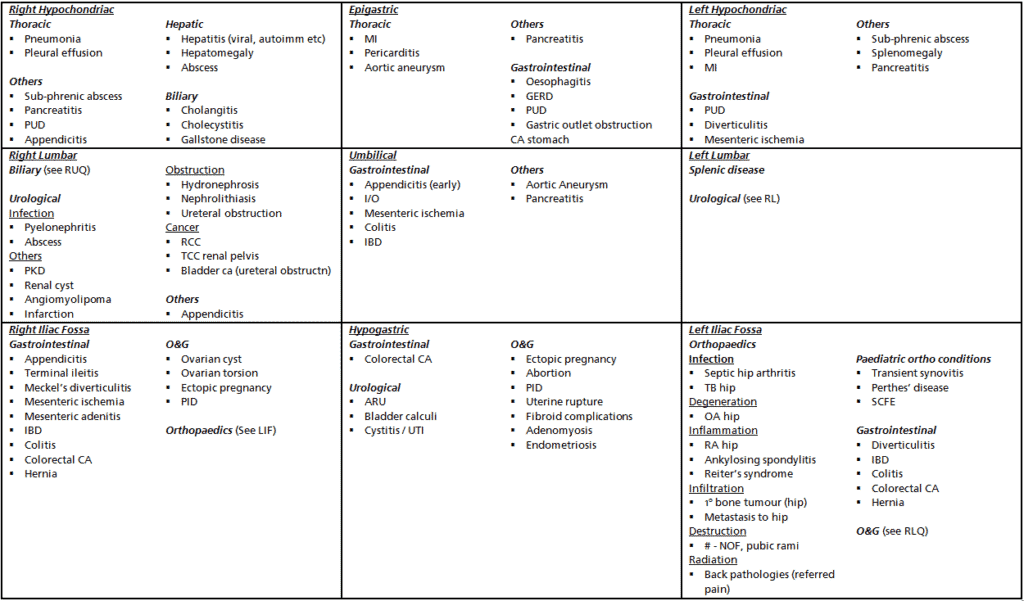
Abdominal pain ddx