Advance Life Support : ECG, Defibrillation, Tachy and Bradyarrythmias Algorithm
Learn how an ECG works, the types and symptoms of arrhythmias, and when defibrillation is needed in cardiac emergencies. A complete guide to heart rhythm care.
Recognising different types of ECG changes is important during resuscitation. This chapter illustrates not only normal sinus rhythm but also include the different types of arrhythmias that may be seen in patients requiring resuscitation.
Isi Kandungan
ALS Core ECG Rhythms & Recognition
1. Normal sinus rhythm

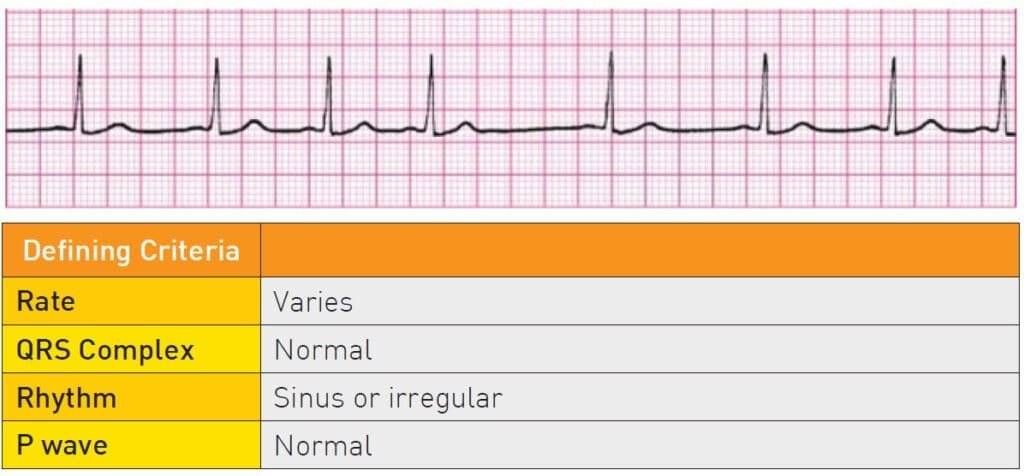
2. Sinus Arryhtmias
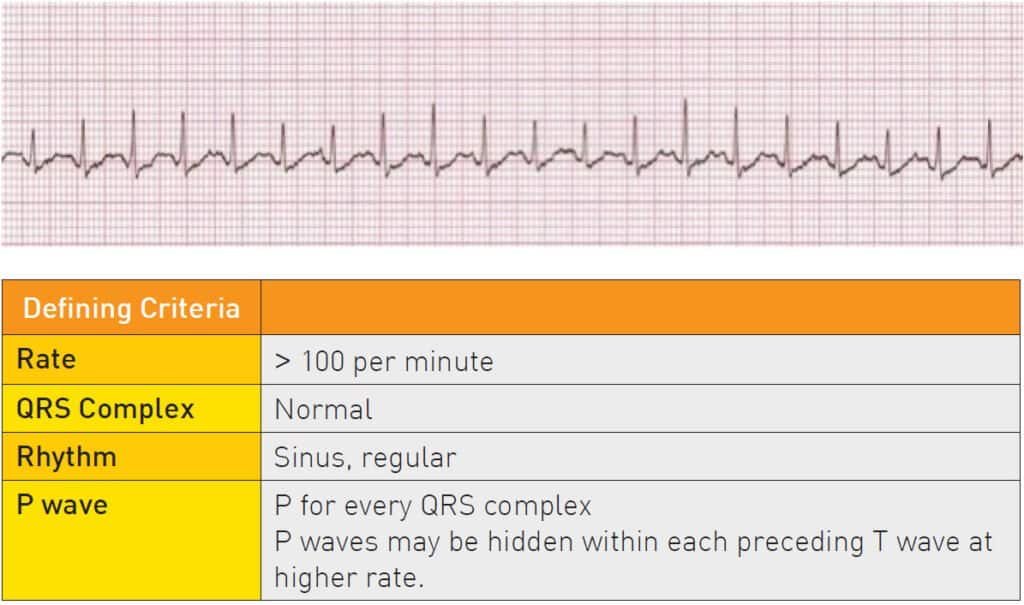
3. Sinus Tachycardia
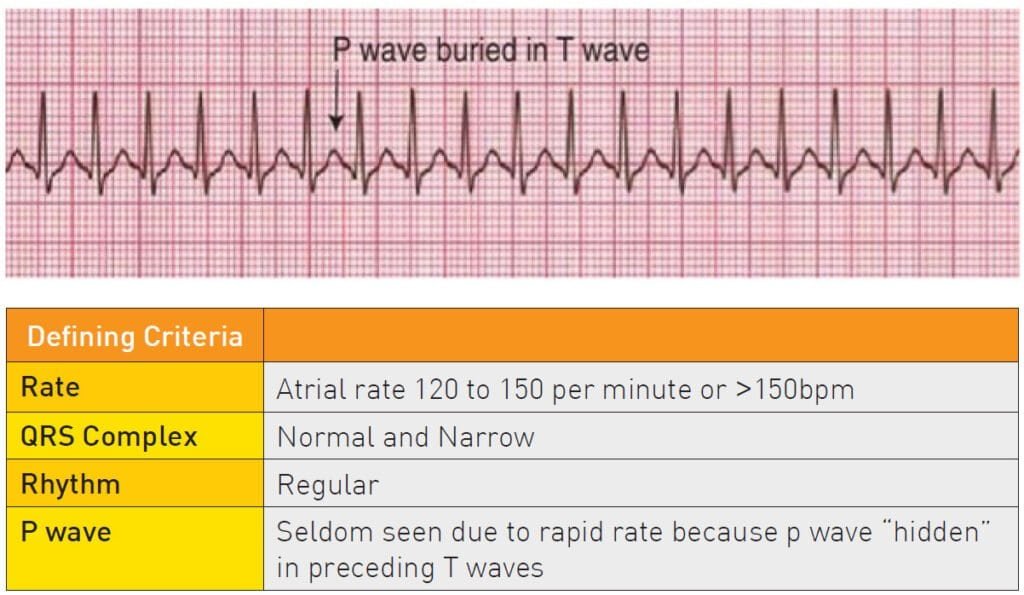
4. Supraventricular Tachycardia (SVT)
5. Sinus Bradycardia

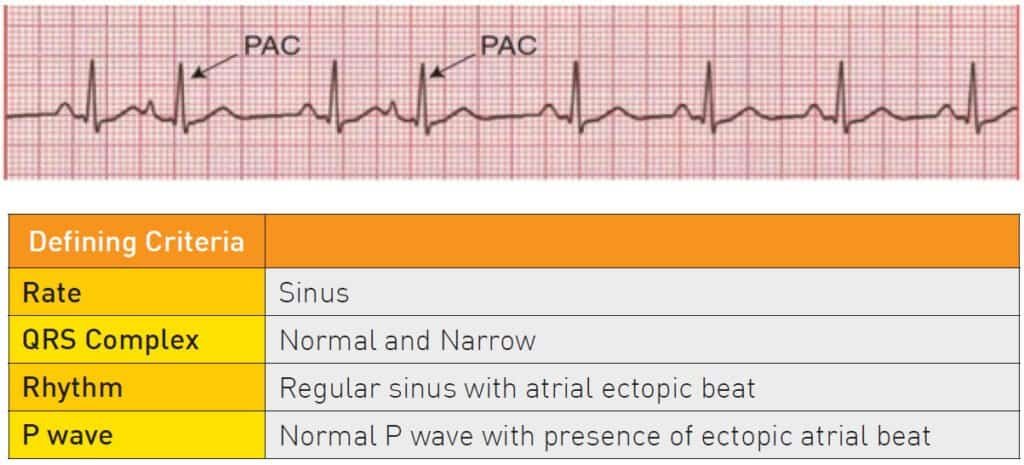
6. Premature Atrial Complexes
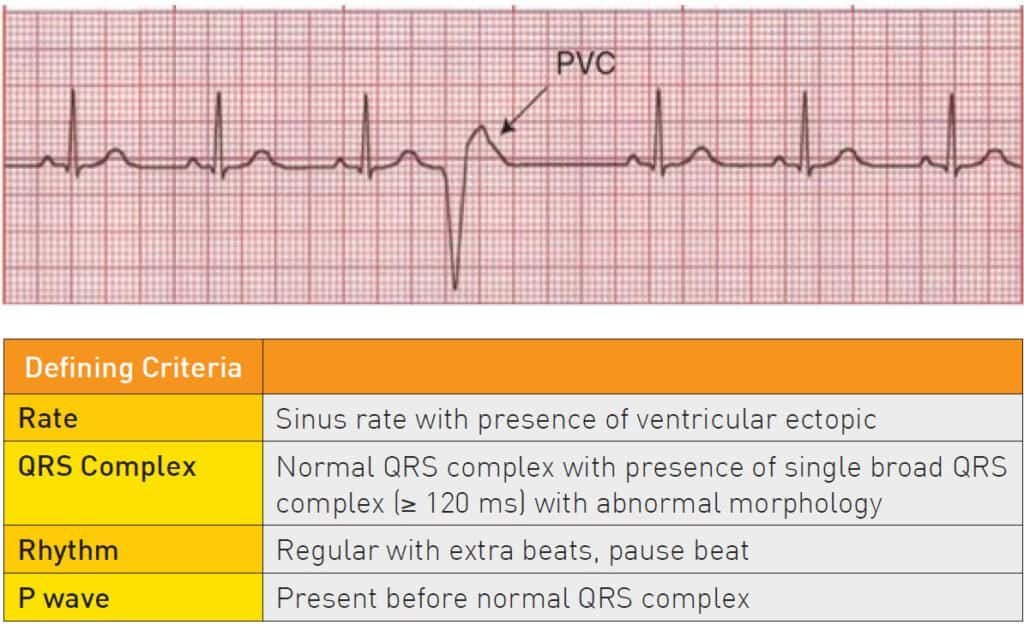
7. Premature Ventricular Complexes (PVCs)
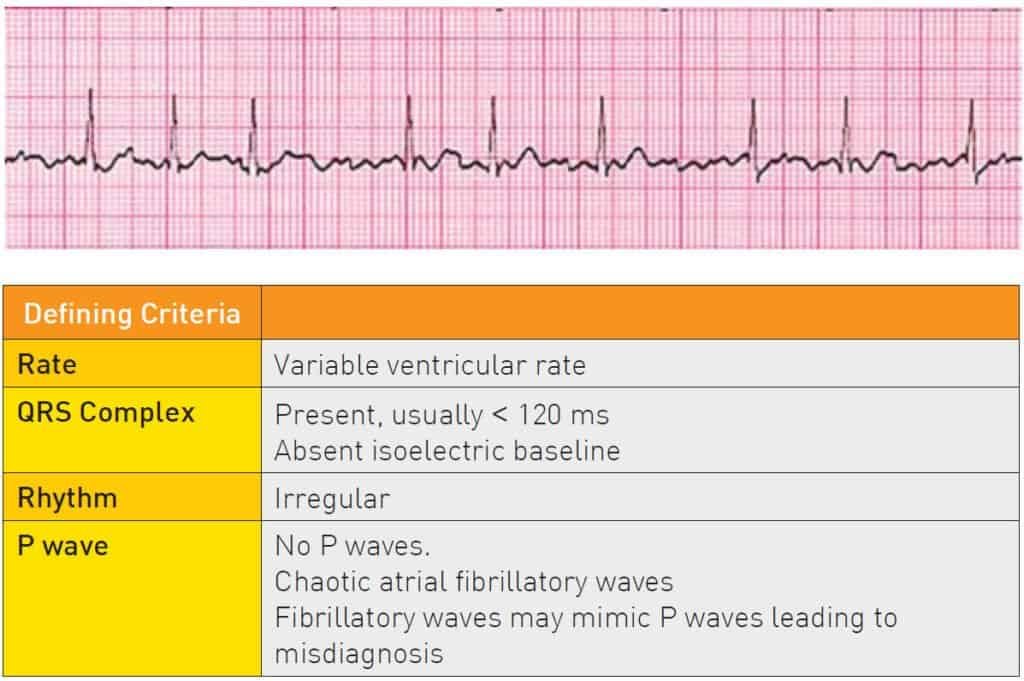
8. Atrial Fibrillation
9. Atrial Flutter

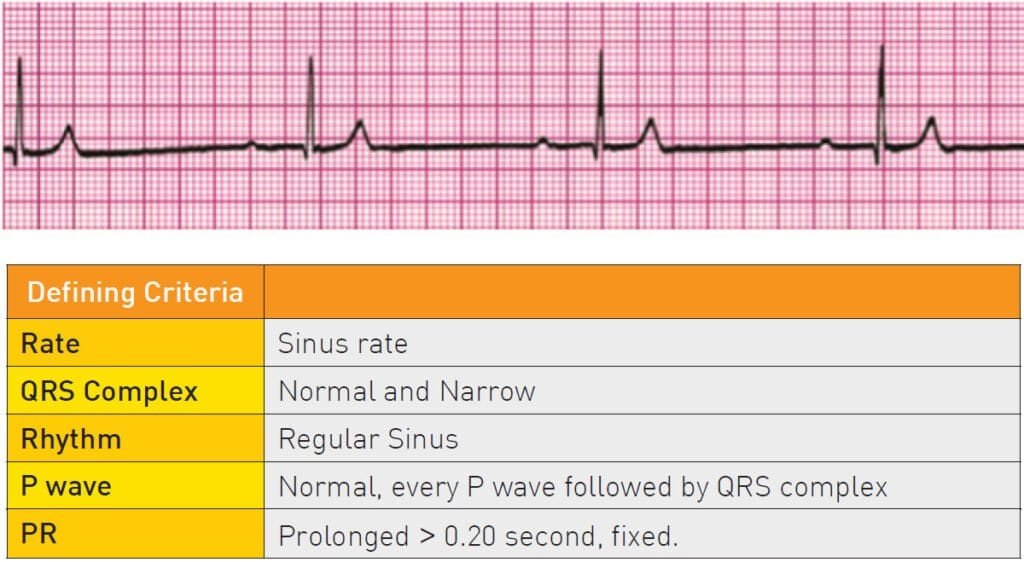
10. 1st degree heart block
11. 2nd Degree AV Block Mobitz Type I (Wenkebach)

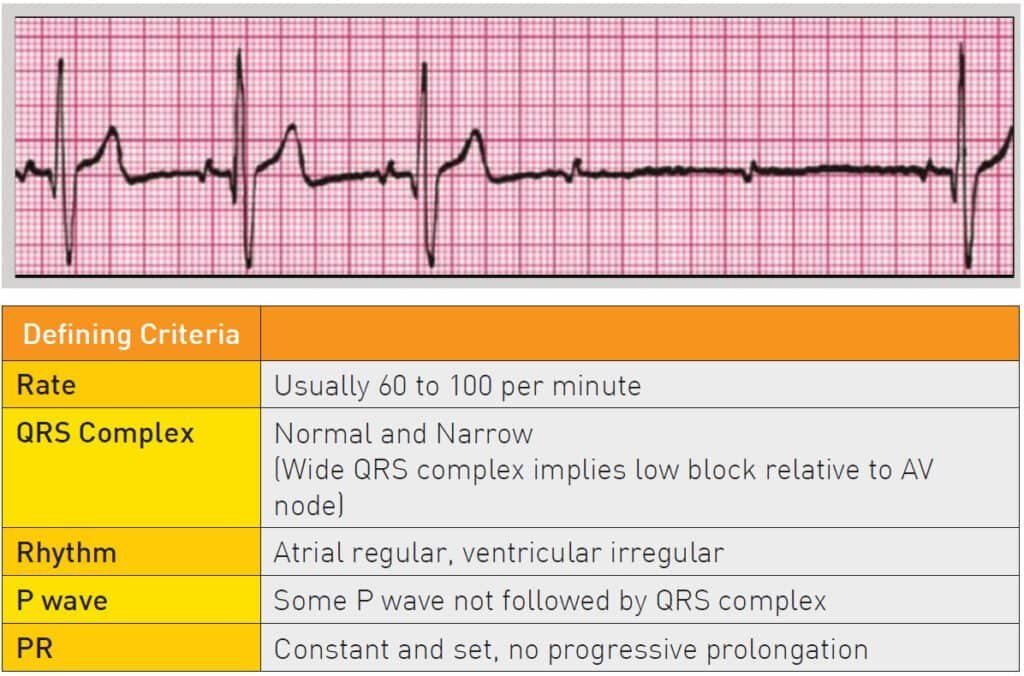
12. 2nd Degree AV Block Mobitz Type II
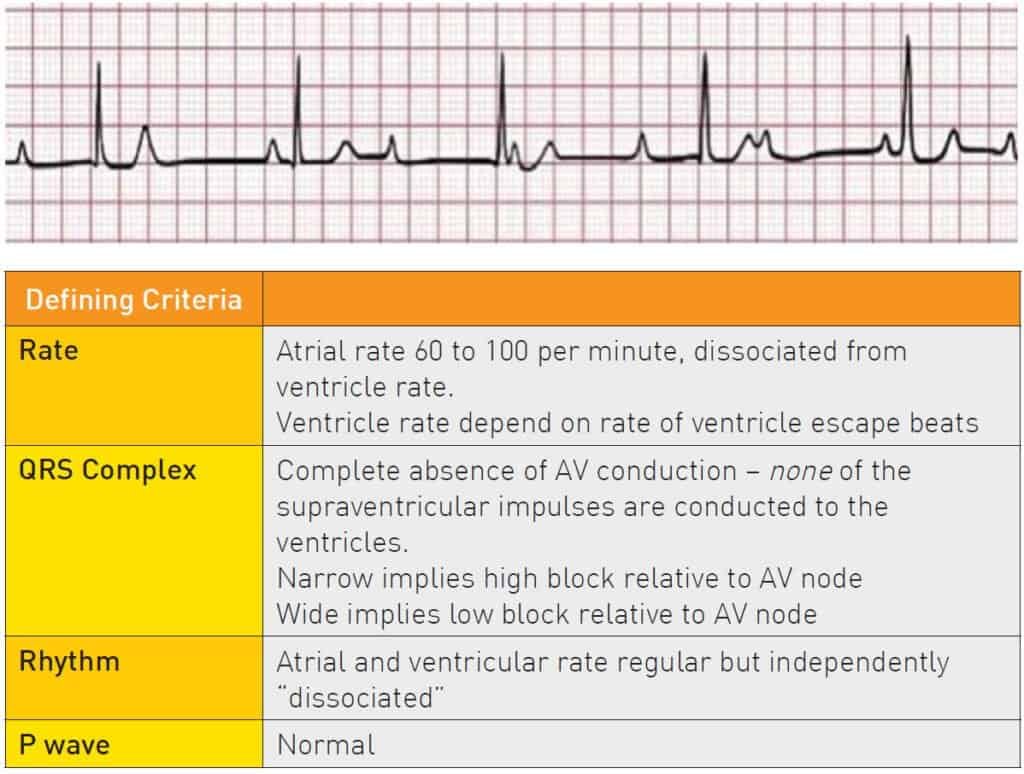
13. 3rd Degree Heart Block
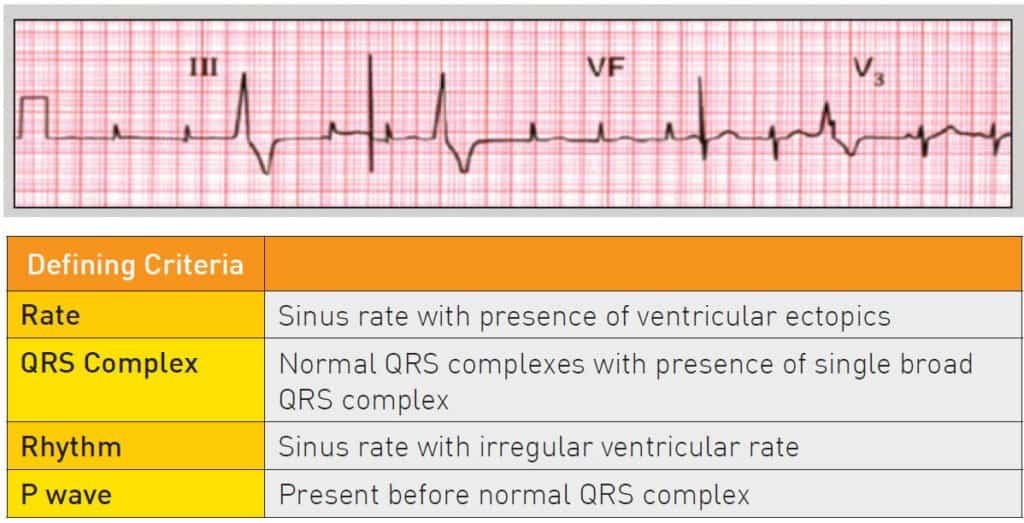
14. Multifocal Ventricular ectopics
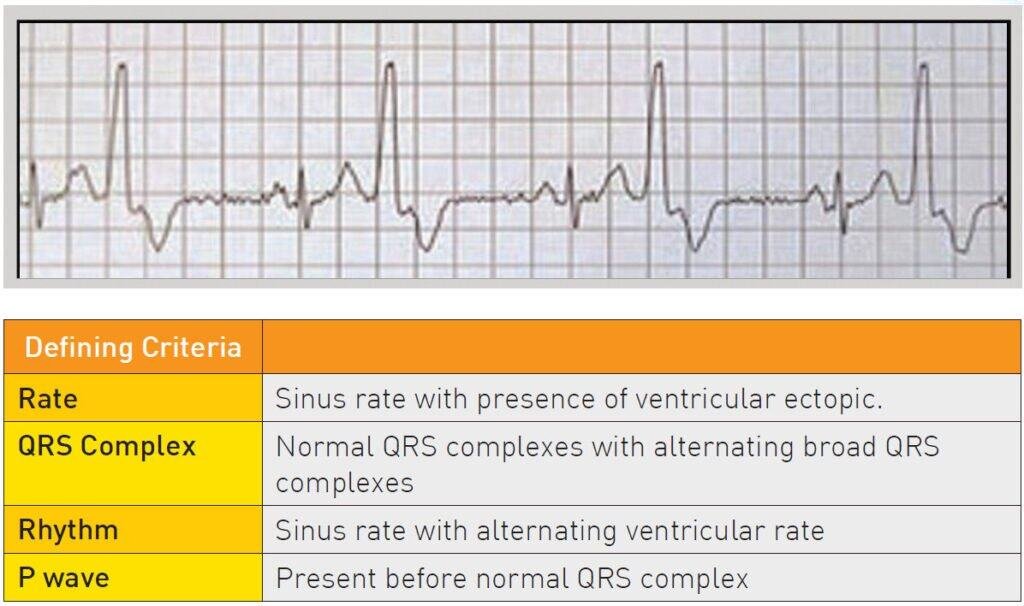
15. Ventricular Bigeminy
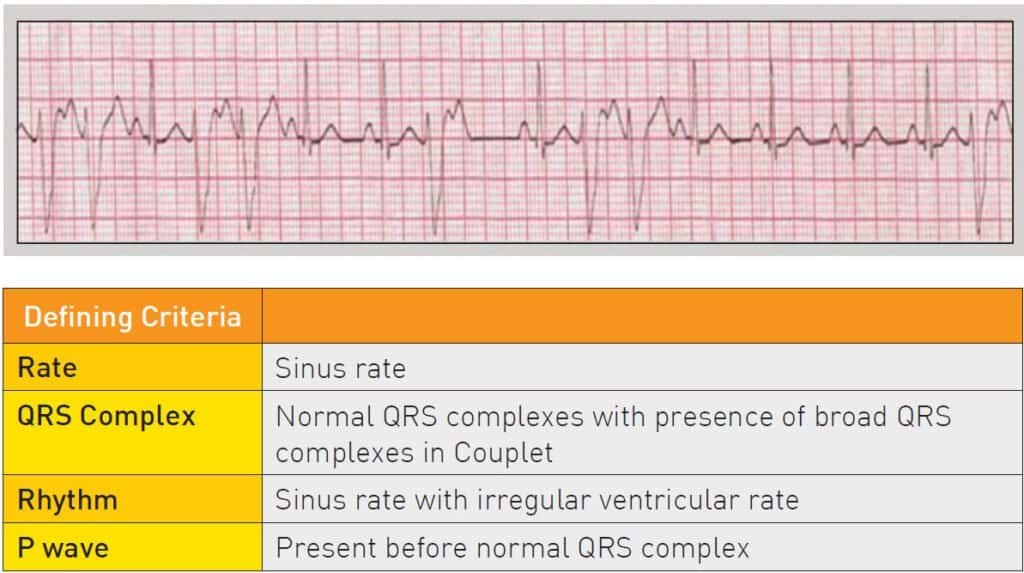
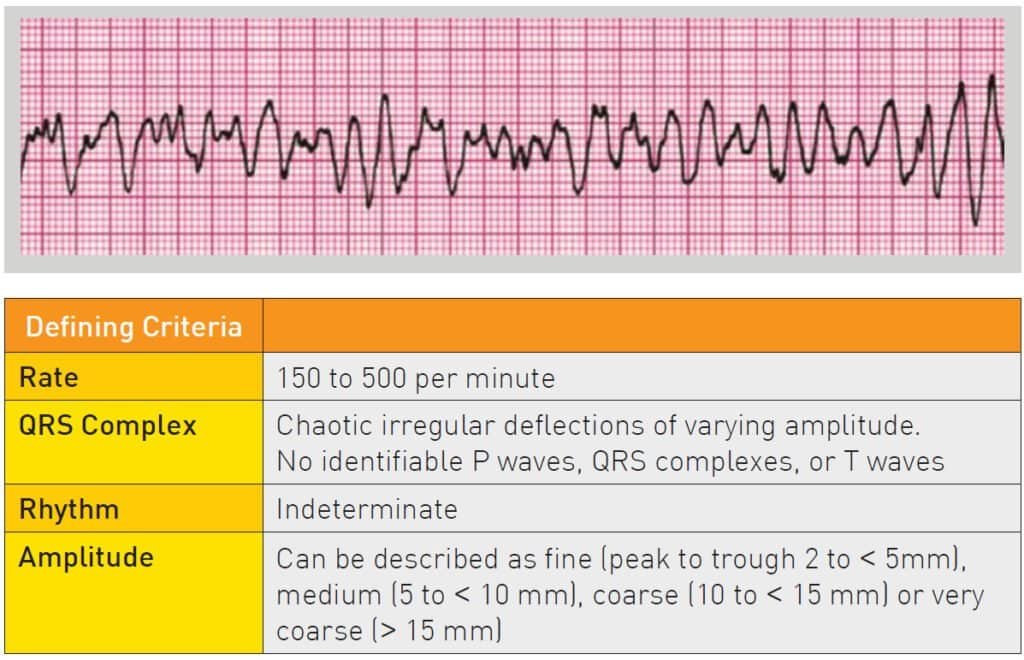
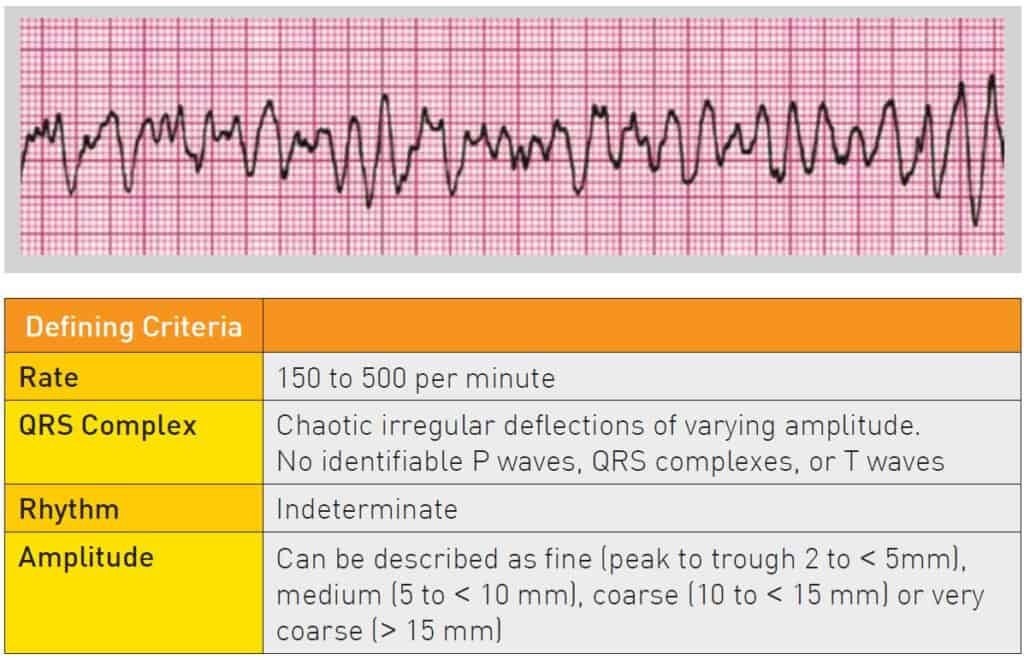
16. Couplets
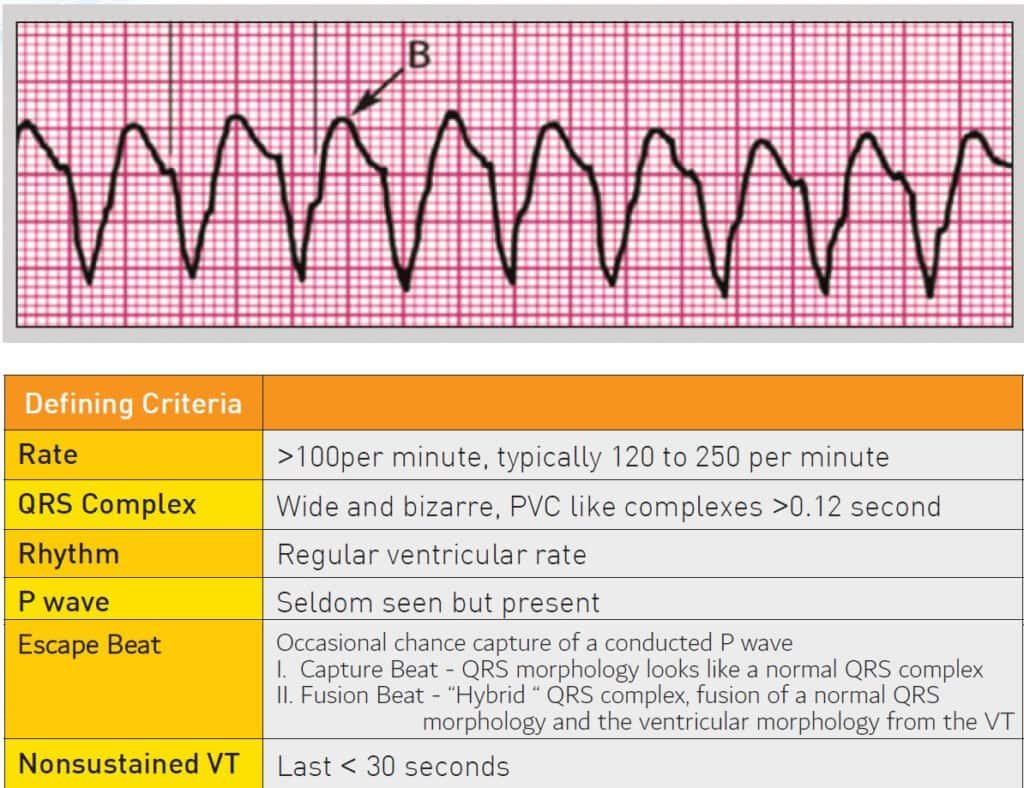
17. Monomorphic VT
18. Polymorphic VT
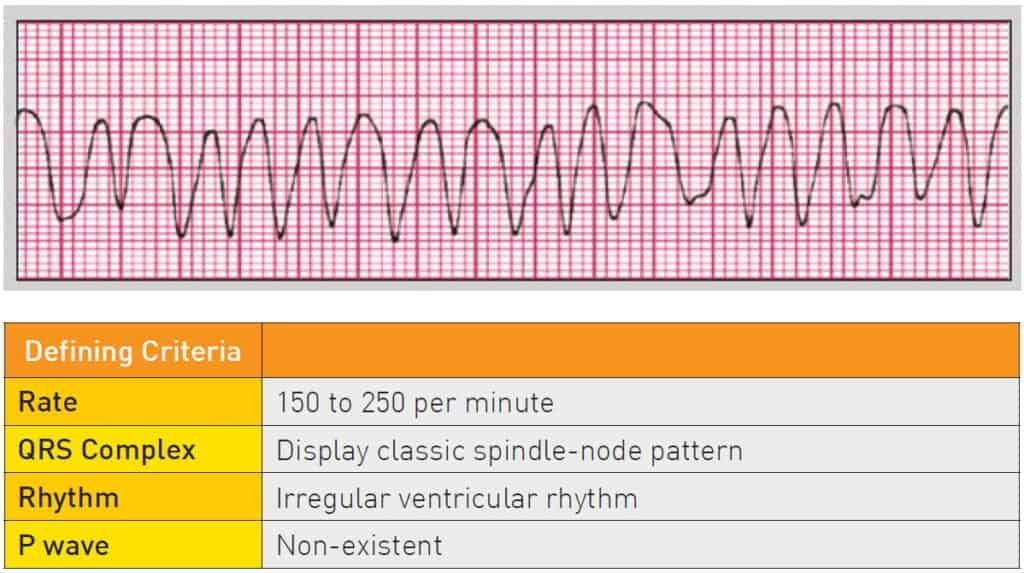
19. Torsades De Pointes

20. Ventricular Fibrillation
21. Asystole
Defibrillation and Electrical Therapy
What is Defibrillation?
- The passage of an electrical current across the myocardium to depolarise a critical mass of myocardium and enable restoration of coordinated electrical activity
- An electrophysiological event that occurs 30-50 ms after shock delivery – the heart is stunned and hopefully the Sino-Atrial (SA) node will take over
- Aims to restore sinus rhythm
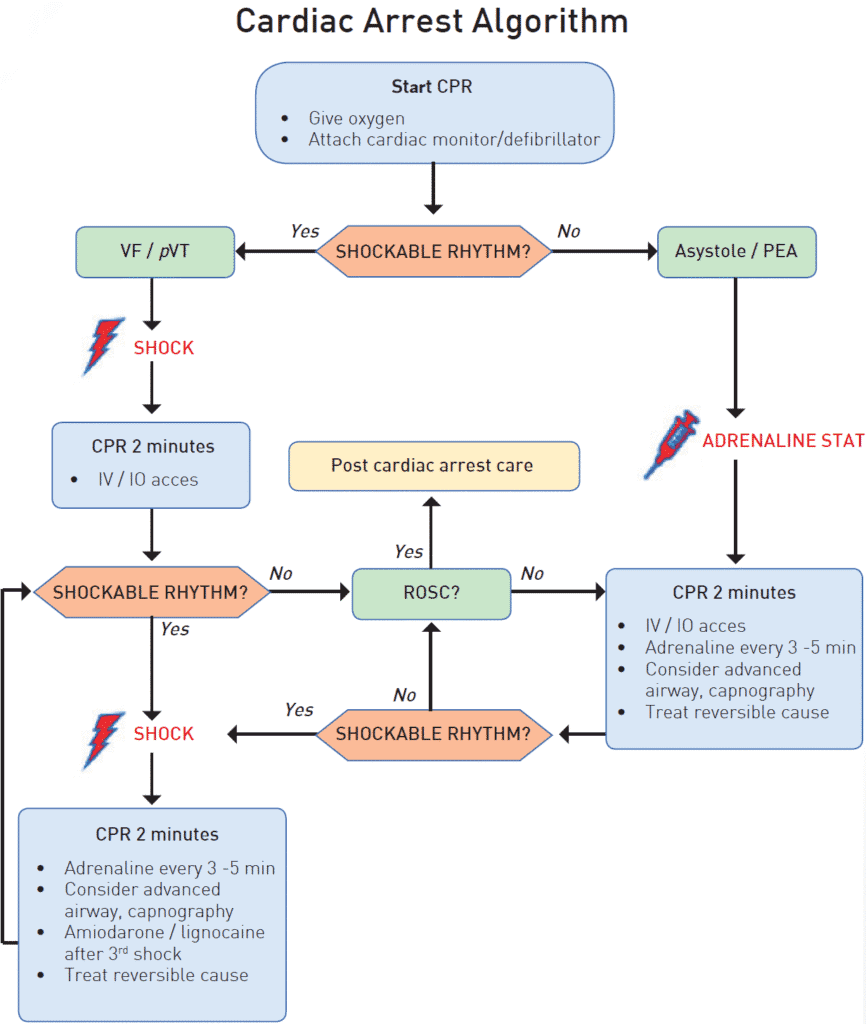
- Indicated only for VF or pVT where a single shock is given followed immediately by chest compression without any pulse check or rhythm reanalysis after a shock
- Shock success typically defined as the termination of VF within 5 seconds after the shock. Shock success using this definition does not equal to resuscitation outcome
The Importance of Early Defibrillation
Early defibrillation is crucial to survival from sudden cardiac arrest (SCA) due to the following:
- Most frequent initial collapsed rhythm in out-of-hospital cardiac arrest (OHCA) is VF
- Defibrillation is the mainstay of therapy to terminate VF
- The probability of successful defibrillation diminishes rapidly over time
- VF tends to deteriorate to asystole over time
Defibrillation should be done without delay when a defibrillator machine is immediately available. Routine delivery of 2 minutes CPR before rhythm analysis and shock for an unwitnessed VF is not recommended.
Defibrillators
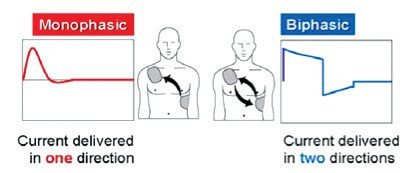
- Modern defibrillators are classified according to 2 types of waveforms: monophasic and biphasic
- Energy levels vary by type of device and manufacturer
- Biphasic defibrillators have greater efficacy in terminating atrial and ventricular tachyarrhythmias.
- Biphasic defibrillators are more commonly used nowadays
Defibrillation energy levels and number of shocks
There is absence of clear evidence regarding optimal initial and subsequent energy levels for shock. Any initial energy level ranging from 120 – 360 J is acceptable, followed by fixed or escalating energy up to the maximum output of the defibrillator.
There remains no evidence to support either a fixed or escalating energy protocol. Both strategies are acceptable; however, if the first shock is not successful and the defibrillator is capable of delivering shocks of higher energy, it is reasonable to increase the energy for subsequent shocks.
A single shock strategy is reasonable in preference to stacked shocks for defibrillation in the setting of unmonitored cardiac arrest. In the setting of monitored cardiac arrest with defibrillator available immediately (during cardiac catheterisation or high-dependency areas), use of up to three stacked
shocks may be considered.
Preparing the Patient
Electrode/Paddle Size
- A larger pad/paddle size (within the limits of 8 – 12 cm in diameter) lowers transthoracic impedance
- Defibrillators with self-adhesive pads have largely replaced defibrillation paddles in clinical practice
Electric/Paddle force
- 8kg force in adult
Transthoracic Impedance
- Use gel pads and electrode paddles or self-adhesive pads to reduce transthoracic impedance
- The average adult human impedance is 70 to 80 Ω. When transthoracic impedance is too high, a low-energy shock will not generate sufficient current to achieve defibrillation
Electrode/Paddle Placement
Anterolateral (sternal-apical) is the position of choice.
— The right (sternal) pad is placed to the right of the sternum, below the clavicle
— The apical pad is placed in the left mid-axillary line, approximately level with the V6 ECG electrode
- Also consider an alternate pad position when the patient is in the prone position (bi-axillary)
- Anterior-left infrascapular, and anterior-right infrascapular electrode placements are comparably effective
- Ensure that the paddle and gel or pads are in full contact with the skin

Special considerations
Breasts
— Place lateral pads/paddles under breast tissue
— Move pendulous breasts gently out of the way
Wet Chest
— Briskly wipe the chest dry before attaching electrode pads and attempting defibrillation
Hirsutism
— Shave hirsute males prior to application of pads
— Remove excess chest hair by briskly removing an electrode pad (which will remove some hair)
— or by rapidly shaving the chest in that area
Automated Implanted Cardioverter Defibrillator (ICD)
— Pad placement to avoid implantable medical devices
— Place the pad away from the device (at least 8 cm) or use an alternative pad position (anterior-lateral, anterior-posterior)
Safety Measures During Defibrillation
- Always announce that a shock is about to be delivered
- Perform a visual check making sure no one is in contact with the patient
- “Clear” the patient and rescuers before each shock
- Remove the oxygen delivery device if in use
- When pressing the shock button, the defibrillator operator should face the patient, not the machine
- A clear and firm warning should be given before delivering a shock (e.g., “Clear shocking”)
- Everyone must stand clear of patient
- The entire sequence should take less than 5 seconds

- Pre shock pause should be no more than 5 seconds. Even a 5 – 10 second delay will reduce the chance of survival. Use of adhesive pad is encouraged to reduce delay
- Continue giving high quality chest compression for 2 minutes after delivery of shock to improve coronary perfusion pressure and cerebral perfusion. Check the pulse and rhythm only after completing 2 minutes of CPR
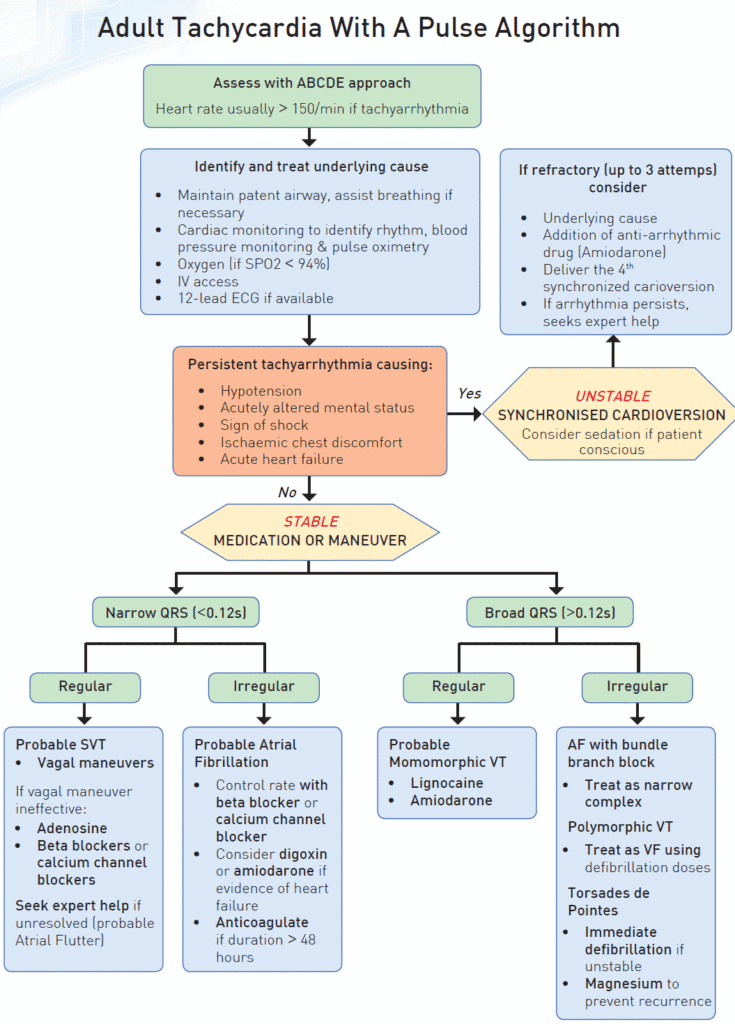
Synchronized Cardioversion
A shock delivery that is timed to occur with the R wave of the electrocardiogram rather than with the T wave
Avoids shock delivery during the relative refractory portion of the cardiac cycle when a shock could produce VF
Use of Synchronized Cardioversion
- Indicated in a hemodynamically unstable patient (low blood pressure) with a perfusing rhythm (pulse present)
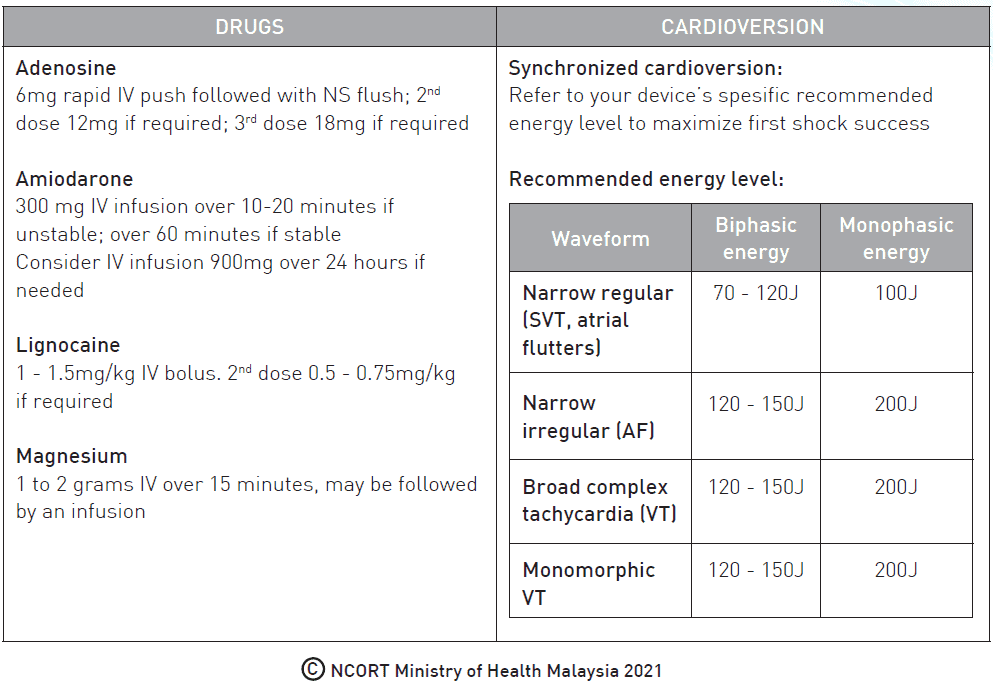
- Recommended in Supraventricular Tachycardia due to re-entry, Atrial Fibrillation, Atrial Flutter and Atrial Tachycardia and Monomorphic VT with pulse
- Conscious patients require anaesthesia or sedation, before attempting synchronised cardioversion

Atrial Fibrillation
- An initial synchronised shock at maximum defibrillator output rather than an escalating approach is a reasonable strategy based on current data
Atrial Flutter and Paroxysmal Supraventricular Tachycardia
- Give an initial shock of 70 -120 J
- Give subsequent shocks using stepwise increase in energy
Ventricular Fibrillation (VF)
- CPR and defibrillation are the mainstay treatment for VF
- Defibrillation as soon as the defibrillator machine is available
- Use of adrenaline after the 2nd shock
- Use of antiarrhythmic after the 3rd shock
- For further details refer to the VF algorithm
Recurrent ventricular fibrillation (refibrillation)
- Recurrence of fibrillation is usually defined as ‘recurrence of VF during a documented cardiac arrest episode, occurring after initial termination of VF while the patient remains under the care of the same providers
- Consider escalating the shock energy after a failed shock
Refractory ventricular fibrillation
- Refractory VF is defined as fibrillation that persists after three or more shocks and occurs in approximately 20% of patients who present in VF
- Consider escalating the shock energy or using an alternative defibrillation pad position (e.g., anterior-posterior)
Patient with witnessed and monitored VF
- In areas where the self-adhesive pads are already attached to the patient e.g., invasive catheterization laboratory, coronary care unit, critical care unit
- 3 quick and successive (stacked) shocks are recommended
- Chest compression is unlikely to improve the already very high chance of ROSC when defibrillation occurs early in the electrical phase, immediately after onset of VF
Ventricular Tachycardia (VT)
If pulseless VT (pVT)
- Treat as VF
Unstable Polymorphic (Irregular) VT
- Treat as VF using defibrillation doses
- Polymorphic VT that occurs in the setting of QT prolongation in sinus rhythm is considered as Torsades de Pointes
- Prompt defibrillation is indicated in patients with hemodynamically unstable Torsades de Pointes
- In the conscious patient with recurrent episodes of Torsades de Pointes, IV magnesium sulfate (initial dose of 1 to 2 grams IV over 15 minutes, may be followed by an infusion) is first-line therapy
Unstable Monomorphic (Regular) VT with a Pulse
- Treat with biphasic waveform cardioversion (synchronized) at 120 J – 150J or monophasic waveform cardioversion at 200 J
- If the initial shock fails, increase the dose in a stepwise fashion
Pacing
- Not recommended for patients in asystolic cardiac arrest as it is not effective and may delay or interrupt the delivery of chest compressions
- It is reasonable for healthcare providers to be prepared to initiate pacing in patients who do not respond to atropine (or second-line drugs if these do not delay definitive management).
- Immediate pacing might be considered if the patient is severely symptomatic
- If the patient does not respond to drugs or transcutaneous pacing, transvenous pacing is probably indicated
ALS Algorithms


Drugs in Resuscitation














Resuscitation in Special Circumstances

Hypoxia
Survival after an asphyxia-induced cardiac arrest is rare and survivors often have severe neurological impairment. Thus, during CPR early effective ventilation of supplementary oxygen is essential. Those who are unconscious but have not progressed to a cardiac arrest are much more likely to make a good neurological recovery. Administer 100% oxygen until oxygen levels can be reliably measured especially at prehospital setting.
Electrolyte imbalances
A high degree of clinical suspicion and aggressive treatment can prevent cardiac arrest from electrolytes abnormalities especially from life-threatening hyperkalemia. Early recognition and prompt treatment must be done immediately and follow standard guidelines for management of hyperkalemia. Other electrolytes disorders are also important to be managed correctly to minimize complications leading to cardiac arrest namely hypercalcemia, hypocalcemia, hypermagnesemia and hypomagnesaemia.
Acidosis
Acidosis is common in cardiac arrest patients. IV sodium bicarbonate (1-2 mmol/ kg) can be considered in presence of severe acidosis.
Hypothermia
Hypothermic patients without signs of cardiac instability (systolic blood pressure 90 mm Hg, absence of ventricular arrhythmias or core temperature > 28o C) can be rewarmed externally using minimally invasive techniques (e.g. with warm forced air and warm intravenous fluid). Patients with signs of cardiac instability should be transferred directly to a centre capable of extracorporeal life support (ECLS). For hypothermic cardiac arrest patients, CPR should be continued during transfer.
Hypovolaemia
Hypovolaemia is a potentially treatable cause of cardiac arrest that usually results from a reduced intravascular volume (i.e. haemorrhage), but relative hypovolaemia may also occur in patients with severe vasodilation (e.g. anaphylaxis, sepsis). Early recognition and immediate treatment with intramuscular adrenaline remain the mainstay of emergency treatment for anaphylaxis. Intravenous adrenaline should only be used by those experienced in the use and titration of vasopressors in their normal clinical practice ( e.g. anesthetists, emergency physicians, intensive care doctors)
Trauma
The mortality from traumatic cardiac arrest (TCA) is very high. Success from resuscitation is time sensitive. The reversible causes in TCA are not the same as cardiac arrest in medical situations. The most common cause of death is haemorrhage. It is recognised that most survivors do not have hypovolaemia, but instead have other reversible causes (hypoxia, tension pneumothorax, cardiac tamponade). Reversible causes should receive immediate and concurrent treatment. Chest compressions should not delay the treatment of reversible causes. Principles of damage control resuscitation in trauma including hypotensive resuscitation, haemostatic resuscitation and damage-control surgery. Cardiac arrest of non-traumatic origin leading to a secondary traumatic event should be recognised and treated with standard algorithms. If available, point of care ultrasound can be used to assist diagnosis, target treatment and assess response.
Tension pneumothorax
Diagnosis of tension pneumothorax in a patient with cardiac arrest or haemodynamic instability must be based on clinical examination. During CPR, presentation is not always classical, but when it is suspected in the presence of cardiac arrest or severe hypotension, chest decompression should be carried out immediately before radiographic confirmation.
Coronary thrombosis
There is limited evidence for recommending the routine transport of patients with continuing CPR after out-of-hospital cardiac arrest (OHCA) of suspected cardiac origin. Transport may be beneficial in selected patients where there is immediate hospital access to the catheterisation laboratory and an infrastructure providing pre-hospital and in-hospital teams experienced in mechanical or haemodynamic support and percutaneous coronary intervention (PCI) with ongoing CPR.
Pulmonary thrombosis
In suspected pulmonary embolism (PE), follow the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) and existing guidelines for PE. Recommendations for administration of thrombolytic drugs when pulmonary embolism is the suspected cause of cardiac arrest remain unchanged. Consider continuing CPR for 60 to 90 minutes after thrombolytic drugs are administered. Routine use of surgical embolectomy or mechanical thrombectomy is however not recommended. Consider these methods when there is a known diagnosis of pulmonary embolism.
Toxins
Ensure personal safety and do not use mouth-to mouth resuscitation in suspected poisoning cases. Routine use of gastric lavage for gastrointestinal decontamination in poisoning is no longer recommended. The preferred method of gastrointestinal decontamination in patients with intact or protected airway is activated charcoal especially if given within 1 hour from the time of ingestion. Reduced emphasis is placed on hyberbaric oxygen therapy in carbon monoxide poisoning. For upto-date guidance in severe or uncommon poisonings, seek advice from a poison centre.