Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis (DKA) is among the most serious acute complications of T2DM
- It has a high mortality rate if unrecognised. The overall mortality is <1%, but a mortality rate >5% in the elderly has been reported.502
- Mortality in patients with DKA is frequently related to the underlying
aetiological precipitant rather than the metabolic sequelae of hyperglycaemia
or ketoacidosis.502
Principles of management
- Correction of dehydration
- Correction of electrolyte imbalance
- Insulin therapy
- Treatment of precipitating factor
- Prevention of complications
Assessment
- Initial assessment
› History and physical examination- Look for precipitating causes: infection, missed therapy, non-adherence,
acute coronary syndrome, cerebrovascular accident, surgery and drugs
(e.g. steroids).
- Look for precipitating causes: infection, missed therapy, non-adherence,
Investigations
- Capillary and venous plasma glucose
- Venous blood gas (pH, bicarbonate)
- Blood or urinary ketones
- BUSE and creatinine
- FBC
- Urinalysis
- If indicated: blood cultures, CXR and ECG
Diagnostic criteria (All 3 criteria must be met)
- Capillary plasma glucose >11 mmol/L
- Capillary ketones >3 mmol/L or urine ketones ≥2+
- Venous pH <7.3 and/or bicarbonate <15 mmol/L
› Patients with high risk for DKA or severe DKA should be admitted to HDU or the ICU. High-risk factors include:
- elderly
- pregnancy
- heart and kidney failure
- other serious co-morbidities
Clinical parameters for severe DKA
– Venous bicarbonate <5 mmol/L
– Plasma ketones >6 mmol/L
– Venous pH <7.1 › Hypokalaemia on admission (<3.5 mmol/L)
– GCS <12
– Oxygen saturation <92% on air (via arterial blood gases [ABG])
– Systolic BP <90 mmHg
– Pulse >100 beats/minute
– Anion gap >16 (Anion gap = [Na+ + K+] – [Cl– + HCO3–])
Treatment
Aims of treatment
– Rate of fall of ketones of at least 0.5 mmol/L/hr, OR
– Bicarbonate rise of 3 mmol/L/hr, AND
– Plasma glucose fall of at least 3 mmol/L/hr, AND
– Maintain serum potassium within normal range.
Precaution during treatment
– Avoid over-correction of hyperglycaemia (within the first 12-24 hours of treatment, avoid lowering glucose to <14.0 mmol/L)
A. Immediate treatment
- Correction of dehydration
› Fluid deficits in DKA may be up to 10% of total body weight. Restoration of circulating volume is a priority.
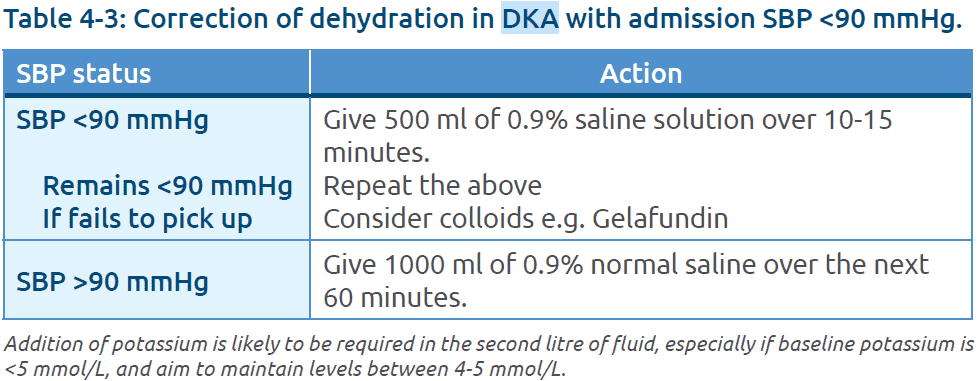
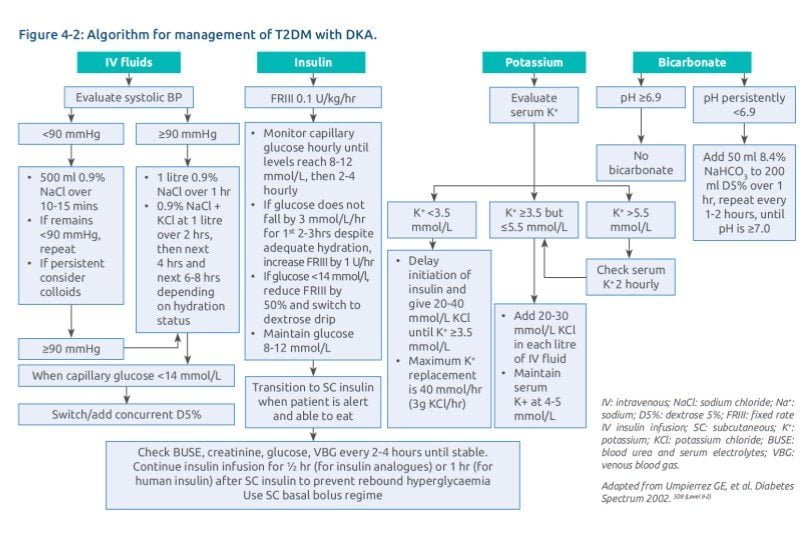
› SBP on admission <90 mmHg (likely due to low circulating volume, but consider other causes such as heart failure or sepsis). Start administration of fluid as shown in Table 4-3.
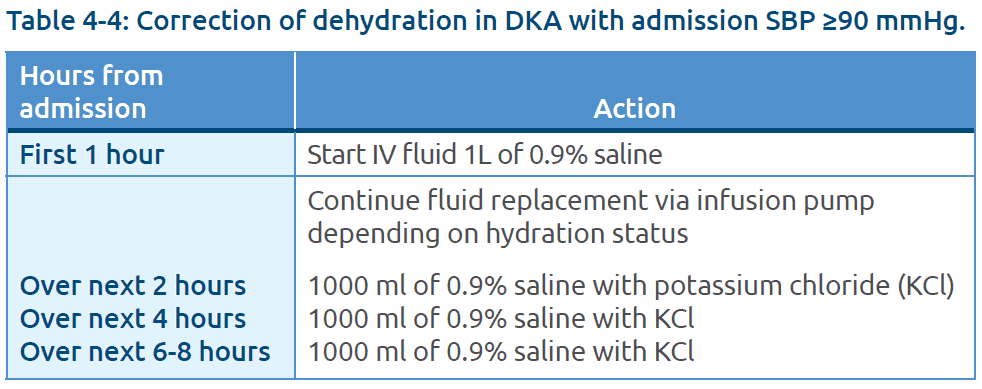
SBP on admission is ≥ 90 mmHg, start administration of fluid as shown in Table 4-4.
- The rate of hydration should be guided by:
- haemodynamic status,
- state of hydration,
- serum electrolyte levels; and
- urinary output.
- More cautious fluid replacement in:**
- young people <18 years
- elderly
- pregnancy
- existing heart or renal failure
** In the above instances, consider HDU admission and, insertion and monitoring via central line.
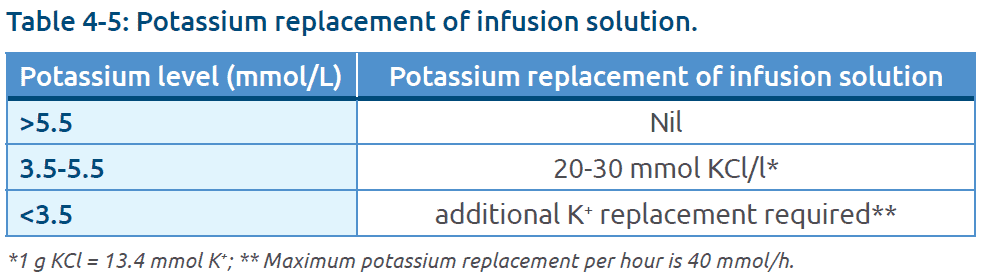
Potassium replacement
› Aim to maintain serum potassium between 4-5 mmol/L.
› Withhold K+ replacement if there is no urine output.
Insulin
› Start a fixed rate IV insulin infusion (FRIII): 0.1 unit/kg/hr based on estimate of weight.
› 50 units short-acting human insulin or rapid-acting insulin analogue made up to 50 ml with 0.9% saline solution.
› Delay insulin infusion if the initial potassium <3.5 mmol/L until serum potassium is corrected.
› Basal insulin – may consider continuing patient’s SC long-acting analogue/human insulin while on IV insulin infusion.
› Monitor capillary glucose hourly – if the glucose does not fall by at least 3 mmol/L/hr in the first 2-3 hours despite adequate hydration, increase FRIII by 1 U/hr.
› Once plasma glucose falls below 14 mmol/L:
– add or switch to 5% dextrose and reduce insulin infusion rate by 50%,
– in the presence of persistent ketonaemia, consider maintaining insulin infusion rate and changing to 10% dextrose.
› Beyond 24 hours, maintain plasma glucose at 8-12 mmol/L.503 (Level III)
IV bicarbonate
› The use of IV HCO3 is not indicated to correct acidosis in DKA due to:
– rise of partial pressure of carbon dioxide (pCO2) in cerebrospinal fluid (CSF) which may lead to a paradoxical increase in CSF acidosis,
– delay in the fall of plasma lactate and ketone level; and
– risk of cerebral oedema especially in younger age group.
› While evidence is lacking, IV HCO3 may be considered if pH is persistently <6.9 despite adequate hydration and insulin treatment.
- E.g. 1 ampoule (50 ml) 8.4% NaHCO3 added to 200 ml D5% over 1 hr, repeated every 1-2 hours, until pH is ≥7.0. Each ml of 8.4% NaHCO3 solution contains 84.0 mg NaHCO3 (e.g. 1.0 mmol/ml).
Phosphate
› No evidence to support routine phosphate replacement for DKA.502 (Level III)
› If levels <0.32 mmol/L in the presence of cardiac dysfunction or respiratory depression, consider phosphate replacement.
B. Monitoring
- Hourly capillary plasma glucose until it reaches maintenance level of 8-12 mmol/L, then monitor 2-4 hourly.
- Vital signs and input-output charting hourly
- Venous HCO3 and K+ at 60 minutes, 4 hours and 6-hourly thereafter
- 6-hourly BUSE and blood/urine ketones
- If ketones and glucose are not falling as expected, check if the insulin infusion pump is working and connected, and the correct insulin residual volume is present.
- If equipment is working but response to treatment inadequate, increase insulin infusion rate by 1 U/hr increments hourly until targets are achieved.
C. Resolution
- Continue IV insulin infusion until resolution of DKA
- Resolution is defined as:
› pH >7.3
› Plasma ketone < 0.6 mmol/L
D. Transitioning from IV insulin to SC basal bolus insulin
- Patient should be eating and drinking, and back on normal insulin.
- Overlap the SC insulin with the insulin infusion for ½ hour (for insulin analogues) or 1 hour (for human insulin).
- Calculating a basal bolus regimen (4 times daily)
- Current practice is shifting away from estimating total daily dose (TDD) of SC insulin based on the last 12-24-hour-insulin administered.
- Estimate total daily dose (TDD) of insulin by multiplying the patient’s weight (in kg) by 0.5 U-0.75 U.
- Use 0.75 U/kg for those considered to be more insulin resistant e.g. obese and/or presence of acanthosis nigricans.
- Give 50% of TDD at bedtime in the form of long acting insulin and divide remaining dose equally between pre-breakfast, pre-lunch and pre-dinner meals.
- For patients already on insulin before admission, consider resuming previous insulin regimen and adjust dose as needed.
- Monitor and adjust insulin doses accordingly.
Reference
CPG Diabetes Mellitus Malaysia